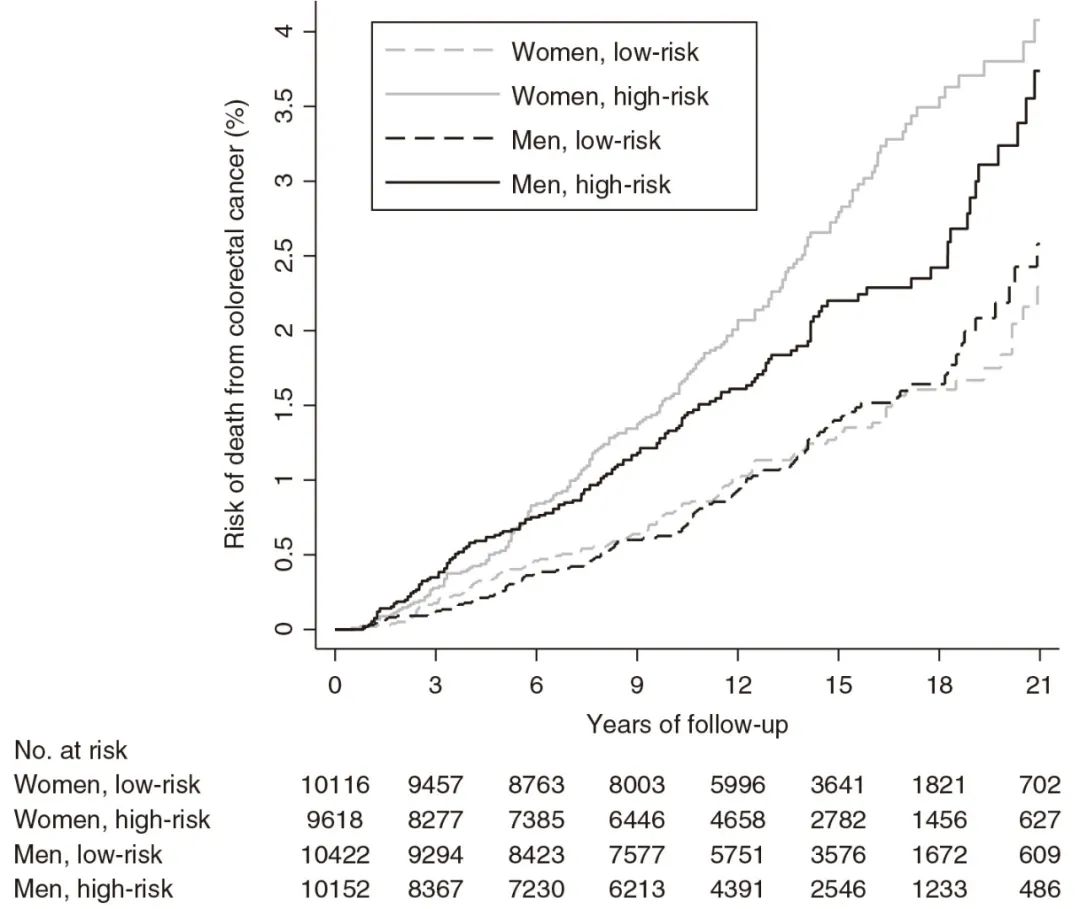
图3 女性和男性在切除低风险和高风险腺瘤后,患结直肠癌的死亡率显著不同。
题目
Long-term colorectal cancer incidence and mortality after adenoma removal in women and men
背景:Women and men with colorectal adenomas are at increased risk of colorectal cancer and colonoscopic surveillance is recommended. However, the long-term cancer risk remains unknown.
目的:To investigate colorectal cancer incidence and mortality after adenoma removal in women and men
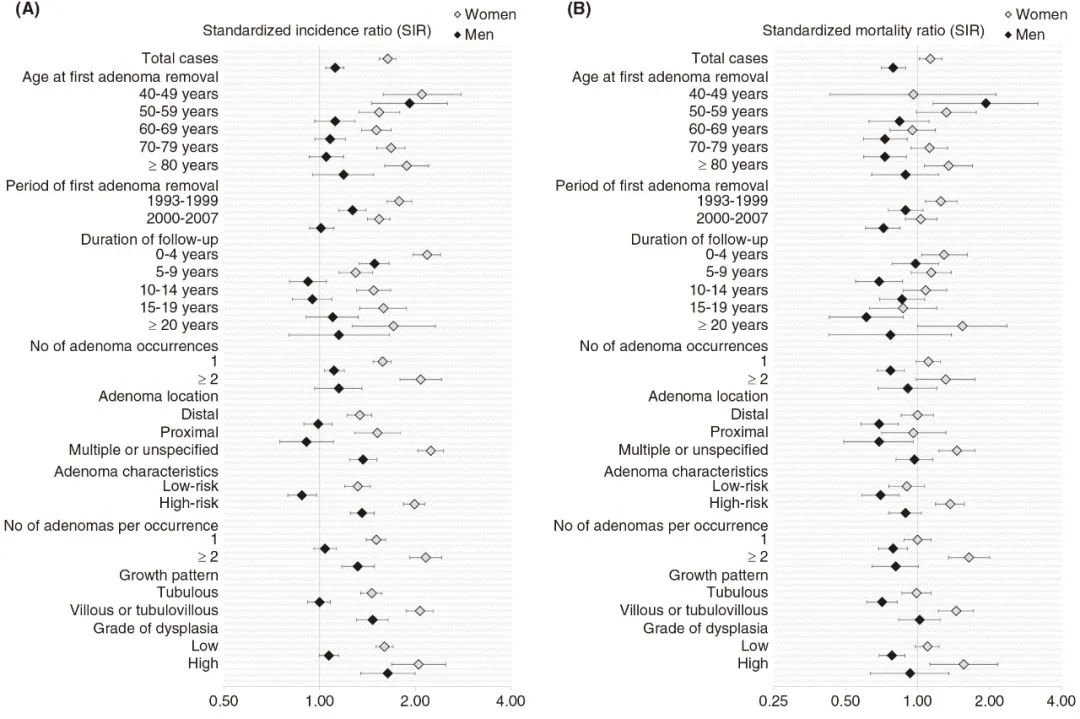
方法:We identified all individuals who had adenomas removed in Norway from 1993 to 2007, with follow-up through 2018. We calculated standardized incidence ratios (SIR) and incidence-based mortality ratios (SMR) with 95% confidence intervals (CI) for colorectal cancer in women and men using the female and male population for comparison. We defined high-risk adenomas as ≥2 adenomas, villous component, or high-grade dysplasia.
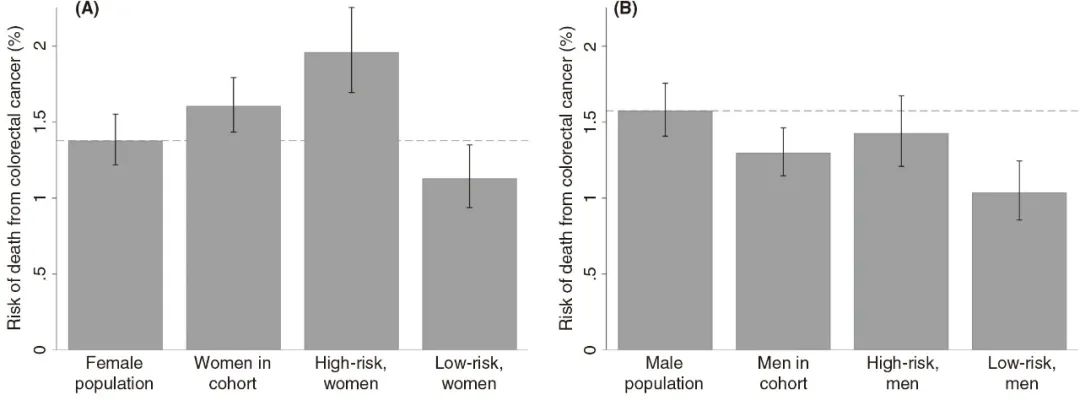
结果:The cohort comprised 40 293 individuals. During median follow-up of 13.0 years, 1079 women (5.5%) and 866 men (4.2%) developed colorectal cancer; 328 women (1.7%) and 275 men (1.3%) died of colorectal cancer. Colorectal cancer incidence was more increased in women (SIR 1.64, 95% CI 1.54-1.74) than in men (SIR 1.12, 95% CI 1.05-1.19). Colorectal cancer mortality was increased in women (SMR 1.13, 95% CI 1.02-1.26) and reduced in men (SMR 0.79, 95% CI 0.71-0.89). Women with high-risk adenomas had an increased risk of colorectal cancer death (SMR 1.37, 95% CI 1.19-1.57); women with low-risk adenomas (SMR 0.90, 95% CI 0.76-1.07) and men with high-risk adenomas had a similar risk (SMR 0.89, 95% CI 0.76-1.04), while men with low-risk adenomas had reduced risk (SMR 0.70, 95% CI 0.59-0.84).
结论:After adenoma removal, women had an increased risk of colorectal cancer death, while men had reduced risk, compared to the general female and male populations. Sex-specific surveillance recommendations after adenoma removal should be considered.