Cancer Metastasis Rev. 2021 Dec 27.
doi: 10.1007/s10555-021-10010-6.
题目
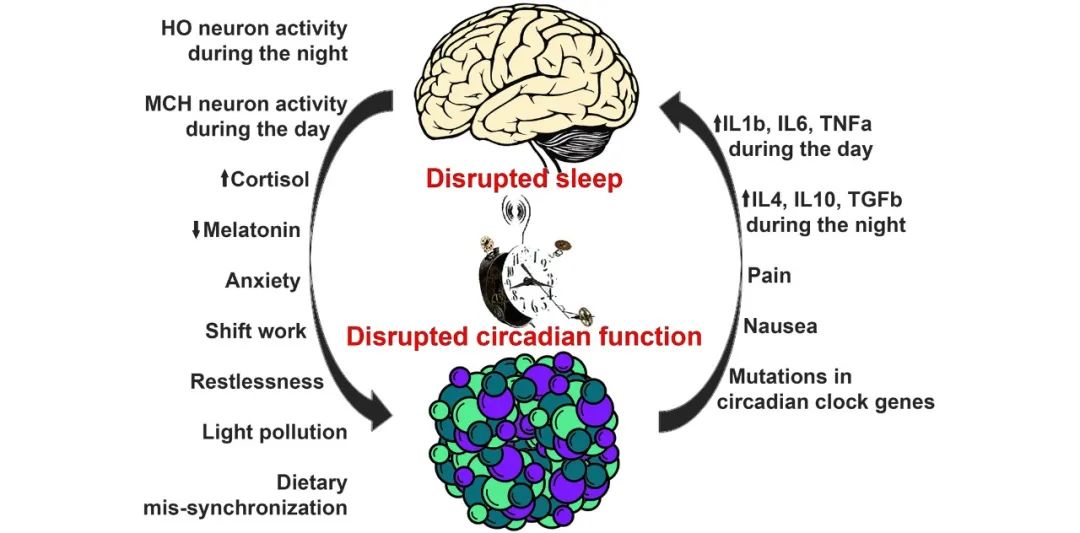
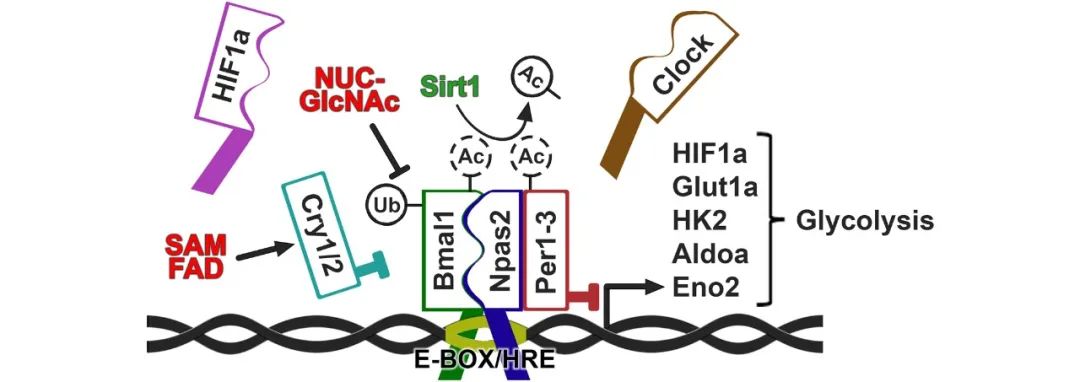
Sleep is a basic need that is frequently set aside in modern societies. This leads to profound but complex physiological maladaptations in the body commonly referred to as circadian disruption, which recently has been characterized as a carcinogenic factor and reason for poor treatment outcomes, shortened survival, and reduced quality of life in cancer patients. As sleep and circadian physiology in cancer patients spans several disciplines including nursing science, neurology, oncology, molecular biology and medical technology, there is a lack of comprehensive and integrated approaches to deal with this serious and growing issue and at best a fractionated understanding of only part of the problem among researchers within each of these segments. Here, we take a multidisciplinary approach to comprehensively review the diagnosis and impact of sleep and circadian disruption in cancer patients. We discuss recent discoveries on molecular regulation of the circadian clock in healthy and malignant cells, the neurological and endocrine pathways controlling sleep and circadian rhythmicity, and their inputs to and outputs from the organism. The benefits and drawbacks of the various technologies, devices, and instruments used to assess sleep and circadian function, as well as the known consequences of sleep disruption and how sleep can be corrected in cancer patients, will be analyzed. We will throughout the review highlight the extensive crosstalk between sleep, circadian rhythms, and metabolic pathways involved in malignancy and identify current knowledge gaps and barriers for addressing the issue of sleep and circadian disruption in cancer patients. By addressing these issues, we hope to provide a foundation for further research as well as better and more effective care for the patients in the future.